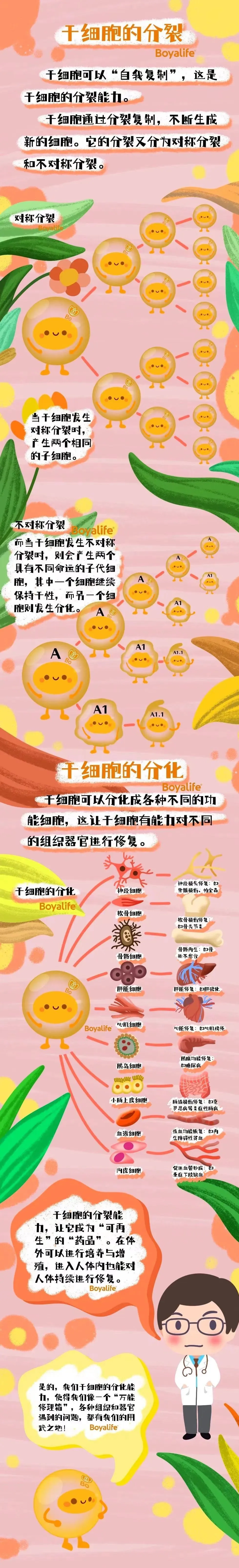
Stem cell transfusion, also known as stem cell transplantation, is a method of obtaining stem cells needed for clinical applications by isolating, purifying, passage, and amplifying cells from various tissue sources in the human body in vitro, and then transfusing them back into the patient's body through intravenous injection or intervention. So why do stem cells transfused back into the body "make up for what is lacking"?
This is mainly due to the homing property of stem cells. When the body is damaged, stem cells will spontaneously go to the damaged area, which is like a GPS installed on the stem cells, which can guide it to its destination at all times-the part of the body that needs to be repaired after damage. In other words, stem cells will "settle down" in the tissue where it is needed.
So, after stem cells "settle down" in a specific location in the human body through homing, what will happen next?
Some people say that stem cells are like Sun Wukong, who can not only transform into 72 different forms by pulling out a hair, but also copy countless of himself. Others say that stem cells are like an elf with powerful magic-self-replication and transformation.
Stem cells can differentiate into various tissue cells, which can make up for aging, death, and damaged tissue cells, so that diseased tissues and cells can recover health. At the same time, stem cells also participate in the repair of new blood vessels and improve the microcirculation of damaged tissues. This is the most basic magic of stem cells.
In addition, after entering the target tissue, stem cells can also secrete many substances that are helpful for human tissue repair, such as proteins, enzymes and various factors.
Through these "magics", stem cells are called the "repair box" of the human body.
With the help of stem cells, the body can easily repair damaged organisms. This is a very important thing that stem cells have to do in the human body after "settling down".
Mesenchymal stem cells are currently the most widely used type of stem cells in clinical practice. They have the ability to self-renew and differentiate into various cell types, and play a key role in immune regulation and regenerative therapy. Mesenchymal stem cells have high-value application potential.
Today, we will take a look at the changes that occur in the human body after the infused mesenchymal stem cells "settle down" in the human body through real clinical cases.
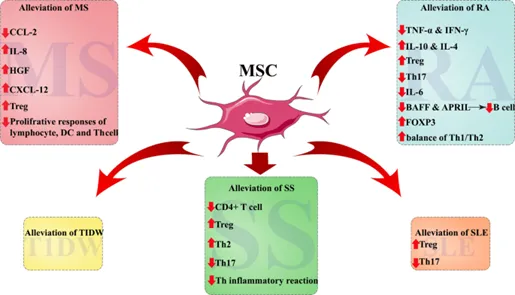
Figure 1: Clinical application of MSCs in disease treatment. [1]
RA, rheumatoid arthritis; T1DM, type 1 diabetes; MS, multiple sclerosis; SLE, systemic lupus erythematosus; IBD, inflammatory bowel disease; SS, Sjögren's syndrome
Reinfused mesenchymal stem cells repair damaged joints
Rheumatoid arthritis (RA), also known as the "immortal cancer", is the most common systemic autoimmune disease in the world, characterized by joint inflammation, synovial hyperplasia, and progressive joint damage, cartilage and bone destruction, and gradually worsens over time, eventually leading to joint deformity and ankylosis. Clinical studies in recent years have shown that more and more patients have had their damaged joints repaired and their symptoms relieved after stem cell infusion.
Research shows that mesenchymal stem cells can reduce the production of pro-inflammatory cytokines such as TNF-α and interferon-γ (IFN-γ), while increasing the secretion of anti-inflammatory cytokines such as interleukin-10 (IL-10) and IL-4 [2]. These characteristics suggest that MSCs may be an emerging therapeutic option for the treatment of RA. Research results also show that MSCs can improve RA through different mechanisms such as inhibiting Th17 cells, reducing inflammatory cytokines, and upregulating Treg cells (see Figure 2) [3].
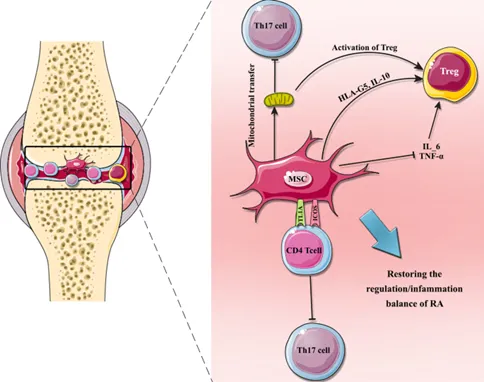
Figure 2: MSCs improve RA by regulating T cells. MSCs can regulate the balance of T cells by homing to the joint cavity and releasing various cytokines that enhance the anti-inflammatory activity of the environment. T cells are also regulated by mitochondrial transfer from MSCs. In addition, the co-stimulatory molecules ICOS (inducible co-stimulator) and TL1A (TNF-like ligand 1A) inhibit Th17 cell differentiation [3].
A 2019 study [4] reported the use of autologous mesenchymal stem cells to treat refractory RA patients. All 9 participants showed improvement in RA symptoms after receiving intravenous injection of 1 × 10^6 autologous MSCs/kg.
In addition, mesenchymal stem cell technology can also be used to target active cells to damaged joints by culturing umbilical cord mesenchymal stem cells with angiogenesis and active tissue repair in vitro, using targeted repair technology. Stem cell repair of arthritis is currently the most sustainable and effective method, which can improve the patient's damaged microenvironment, regulate immune function, and activate damaged and dormant cells. After activation, the cells can grow, proliferate, and repair damaged tissues in the body, prevent further damage to joint structures, and inhibit abnormal immune functions, thereby curbing the development of complications and restoring normal functions of the body.
In summary, these data show that MSC cell therapy is a hope for the clinical treatment of RA, which can significantly improve patients' clinical symptoms and effectively prevent disease progression.
Reinfused stem cells, rebuild endogenous insulin secretion function
Type 1 diabetes (T1DM) is a group of autoimmune diseases in which autoreactive immune cells lead to complete insulin deficiency[6]. Type 1 diabetes is a chronic disease in which the body's own immune cells attack and destroy pancreatic β cells. Once β cells are destroyed, the pancreas will no longer produce insulin.
Stem cells can regulate the imbalanced immune system and differentiate into islet-like secretory cells to re-establish the endogenous insulin secretion function and restore blood sugar to normal.
Stem cells have strong proliferation ability and the potential to differentiate into insulin-secreting cells, which can replenish the number of pancreatic β cells for the body and rebuild the endogenous insulin secretion function. By transplanting stem cells that are induced to differentiate into pancreatic cells, damaged pancreatic cells can be replaced to secrete insulin, thereby improving diabetes and significantly reducing the use of hypoglycemic drugs.
In addition, stem cells can also improve the body's sugar metabolism function, effectively lower blood sugar levels, and play a role in improving and preventing diabetes. Stem cells have immunomodulatory or immunosuppressive effects on T cells, B cells, dendritic cells and NK cells, and can protect pancreatic β cells and reduce damage caused by autoimmunity. A large number of studies have shown that stem cells have a relieving effect on chronic inflammation and can improve insulin resistance.
In addition, stem cells have the ability to home to damaged tissues. They can migrate to damaged pancreatic islet cells, paracrine and autocrine a variety of active cytokines and growth factors, participate in the repair of pancreatic islet cells, and promote the regeneration of pancreatic β cells. Stem cells can also promote the transdifferentiation of pancreatic α cells to β cells.
In 2016, the literature [8] randomly performed UC MSCs transplantation on 42 patients with T1DM. Within 1 year after treatment, the patients' fasting blood sugar decreased and their daily insulin requirements decreased. Based on these results, it can be seen that UC-MSC therapy is safe and can improve the symptoms of T1DM patients.
Reinfused stem cells regulate disordered autoimmune function
Systemic lupus erythematosus (SLE) is a chronic inflammatory autoimmune disease that causes antibody-antigen immune complexes to deposit in various organs[12]. It can be said that systemic lupus erythematosus is a disorder of the patient's immune function, with a large amount of autoantibodies and immune complexes produced, causing damage to multiple systems and organs.
Stem cells have the potential to regulate disordered autoimmune function, and its mechanism mainly includes the following aspects:
Immunomodulatory effect: Stem cells can secrete anti-inflammatory factors and immunomodulatory factors to inhibit the overactivation of immune cells and inflammatory response, thereby regulating disordered autoimmune function.
Promote the differentiation of immune cells: Stem cells can differentiate into immune cells, such as dendritic cells, macrophages, etc. These cells can further regulate immune responses, thereby restoring the balance of the immune system.
Regulate T cell function: Stem cells can regulate T cell function, promote T cell differentiation and proliferation, and inhibit T cell overactivation, thereby alleviating the symptoms of autoimmune diseases.
Promote immune cell homeostasis: Stem cells can promote immune cell homeostasis, that is, inhibit the overactivation and attack of autoimmune cells, thereby reducing the occurrence of autoimmune diseases.
In 2014, the Drum Tower Hospital Affiliated to Nanjing University Medical School [13] conducted a clinical trial on 40 patients with active and refractory SLE. After UC-MSC infusion treatment, the patients' observations showed a significant decrease in SLEDAI and BILAG scores as well as proteinuria, serum creatinine and urea nitrogen. At the same time, serum albumin and complement concentrations increased, and no adverse events related to administration were shown, and all participants were able to tolerate the intervention treatment well.
In addition, the Drum Tower Hospital affiliated to Nanjing University Medical School [14] also conducted a study in 2016 to evaluate the safety of allogeneic UC-MSC in the treatment of refractory SLE patients. UC-MSC were intravenously injected into 9 SLE patients on days 0 and 7. After 6 years of follow-up, no side effects such as headache, nausea or vomiting were observed in these patients.
Reinfused stem cells repaired the inflamed intestine
Inflammatory bowel disease (IBD) is a chronic inflammatory gastrointestinal and autoimmune disease, including ulcerative colitis (UC) and Crohn's disease (CD). IBD is mainly caused by inappropriate and persistent immune responses of genetically susceptible hosts to pathogenic microorganisms [23].
Stem cells can repair damaged intestines, and their mechanisms mainly include the following aspects:
Differentiation into intestinal cells: Stem cells have multi-differentiation potential. Under appropriate conditions, they can differentiate into intestinal cells and replace damaged intestinal cells, thereby restoring the normal function of the intestine.
Secreting anti-inflammatory factors: Stem cells can secrete anti-inflammatory factors, inhibit intestinal inflammatory reactions, reduce intestinal mucosal damage and inflammatory cell infiltration.
Promote intestinal mucosal repair: Stem cells can promote the proliferation and differentiation of intestinal mucosal cells, thereby accelerating the repair and regeneration of intestinal mucosa.
Regulate the intestinal immune system: Stem cells can regulate the function of the intestinal immune system and promote intestinal






